Reimagining Northwestern Medicine’s caregiver education procedures to improve long-term health outcomes.
Service Design, Healthcare DesignMarch 2021 - June 2021
My Responsibilities: Conducting problem space identification, conducting stakeholder interviews, creating service blueprint, creating storyboards, communicating with partners at Northwestern Medicine, presenting findings to a team of clinicians
Deliverables: Service blueprint, caregiver journal, clinician checklist, revised hospital protocol, slide deck
Overview
As part of a self-guided group independent study research project, my team and I delved into the space of CAR-T cell therapy, a space I discovered in the early stages of working on Hearth Health. Our investigation started out broadly, interviewing expert stakeholders across a variety of touchpoints in CAR-T cell therapy supply chain (clinical trials, manufacturing, and academic research). We formed a partnership with Northwestern Medicine’s CAR-T Cell Therapy treatment program, who were beginning the process of developing an outpatient treatment model. Administering CAR-T cell therapy in an outpatient setting increases reliance on home caregivers, which led us to focus on improving the education and resources provided to caregivers. Our prototypes and recommendations were incorporated into Northwestern Medicine’s treatment procedures to be tested in a dry run of the outpatient treatment program.
Opportunity
At the outset of this project, Northwestern Medicine only offered CAR-T cell therapies in an inpatient setting due to a variety of potentially fatal side effects which necessitate 24-hour monitoring. However, Northwestern Medicine wanted to start offering CAR-T cell therapies in an outpatient setting. As therapies are being approved for new cancers, the number of patients seeking CAR-T therapies from Northwestern Medicine is increasing rapidly. However, the Northwestern Medicine team did not have space in the hospital to account for this increase in patients, considering that patients stay in the hospital for two weeks post infusion. To increase the number of patients the hospital was able to treat, there was a clear need to develop an outpatient treatment protocol.
When considering what was needed to adapt their inpatient protocol to an outpatient one, one area of need emerged: due to an increased reliance on untrained family members as caregivers for 24-hour care, the ways in which Northwestern Medicine was educating and preparing them needed to improve.
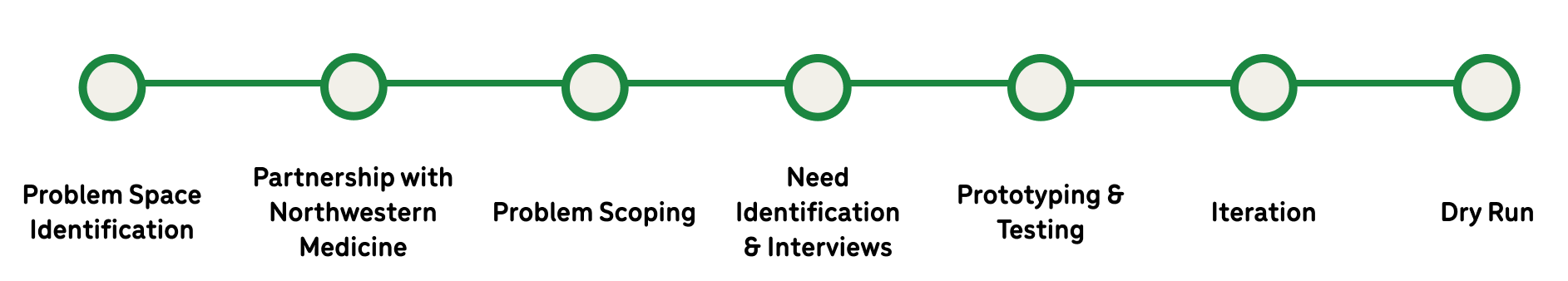
Process
Problem Space IdentificationPrior to forming our partnership with Northwestern Medicine, we researched the space of CAR-T cell therapy broadly by conducting extensive literature reviews, and talking with industry experts who work for drug manufacturers as well as clinicians administering therapies. One such conversation was with the clinical head of Northwestern Medicine’s CAR-T Cell Therapy program.
Partnership with Northwestern MedicineAfter interviewing the clinical director of Northwestern Medicine’s CAR-T Cell Therapy program, it was clear that they had a variety of potential areas for improvement which would benefit from my team’s human centered design skills. Once we had a set of problems to investigate, the fun could really begin.
Problem ScopingAfter establishing our partnership with Northwestern Medicine, we began speaking to various clinicians and staff members on their team to identify potential areas for process improvement. Three key areas for potential improvements emerged:
We discussed further with our partners at Northwestern Medicine to prioritize these needs. Northwestern Medicine was in the process of creating a protocol for administering therapies in an outpatient setting, and we quickly realized the importance of the first two problem spaces in an outpatient setting. Due to the increased reliance on family caregivers in an outpatient setting, we focused on improving communication between clinicians and patients and their family members. This led us to our guiding question:
How might we educate caregivers such that they feel more confident and prepared to care for CAR T-cell therapy patients in an outpatient setting?
Need Identification & InterviewsTo better understand the current process for inpatient care which was to be adapted to create an outpatient treatment process, we created a preliminary service blueprint of the inpatient treatment process.
We combed through this blueprint to identify key areas to discuss with our clinical partners.
After discussing and ensuring we understood all touchpoints, we came up with a mockup of a timeline for outpatient care. We presented this simplified timeline as a stimulus for further interviews with clinical staff, and had them place different information that needed to be covered into different appointments, to get a sense of what the “ideal” timeline for education would look like.
Additionally, we created very rough storyboards depicting potential additions to the education process. These were based on preliminary hypotheses we had about potential gaps in the education process. We presented these to clinicians as well as to the caregiver we were able to interview. We kept these storyboards low fidelity, so all our interview subjects were comfortable giving feedback.
We had the opportunity to interview a caregiver whose husband received CAR-T cell therapy from Northwestern Medicine right at the onset of the COVID pandemic. The caregiver we interviewed was a retired nurse, who was able to rely on her clinical training to improve the care she provided her husband. While she was overwhelmed by the tasks she had to do once her husband returned home a month after receiving treatment, she was able to use her know-how as a nurse to work around some of these problems. Uncovering the work arounds she used was an “a-ha” moment for our team that directly impacted the solutions we created for Northwestern Medicine.
Through our interviews with clinical staff and the caregiver, we identified three key areas of need to support caregivers:
Prototyping and TestingAfter identifying key areas of need, we began prototyping solutions by creating refined storyboards. We solicited feedback on two distinct solutions: an education touchpoint checklist and instructional videos to be used by caregivers once they have returned home.
We sent these storyboards to the clinical care team at Northwestern Medicine to get their feedback, trying to understand what educational touchpoints should be reviewed in the checklist and videos. We synthesized these ideas in Mural:
Final DeliverablesAfter synthesizing feedback from clinicians, we created final prototypes to be used in Northwestern Medicine’s upcoming dry run of their outpatient treatment process. These included: a service blueprint, a caregiver journal, an education checklist, and finally instructional videos and corresponding changes to Northwestern Medicine’s CAR-T landing page.
Service Blueprint
After making a rough blueprint of the inpatient care model as depicted above, we created a service blueprint of the outpatient care model. In this blueprint, we chose to highlight education touchpoints, location of patient and caregiver, and role of clinicians in these steps.
The blueprint was used as a clear visual aid to help communicate the importance of these interactions in a clear and easily digestible way.
To be of most use to Northwestern Medicine’s care team, we also put this information into their working outpatient workflow prototype in PowerPoint.
Caregiver Journal
Based on our conversations with caregivers and clinicians, we created a detailed journal to be used by caregivers as they monitor the patient from home. We included sections for vital sign recording, medication administration records, and handwriting checks as a form of assessing mental acuity.
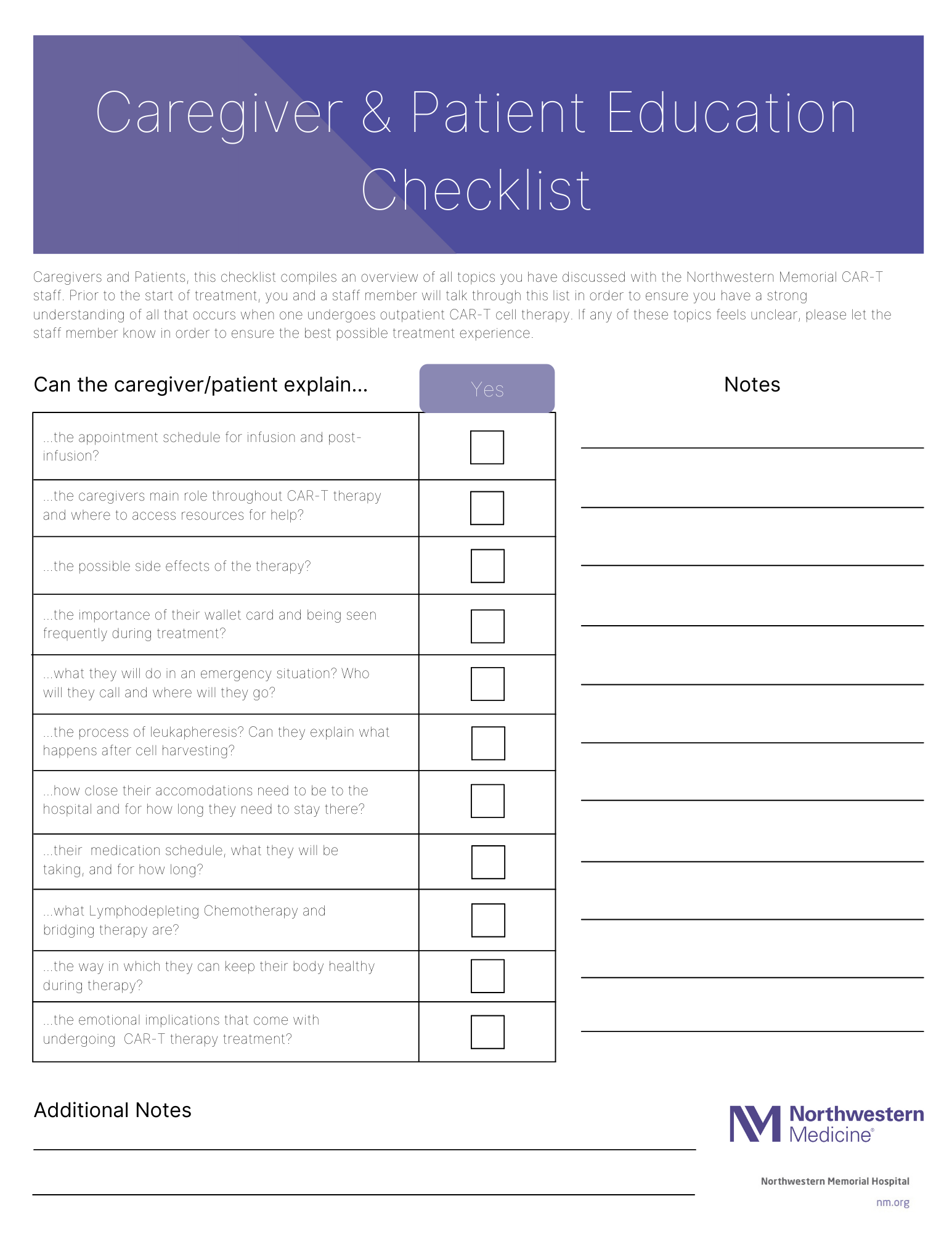
Education Checklist
Our research revealed that there was no standardized way for recording which information has been taught to patients and their caregivers, meaning that some information is often repeated or omitted during the appointments preceding the patients’ procedures. To address this, we created a checklist of key educational areas which must be covered, so that information can be standardized across the clinical care team.
Instructional Videos
We heard that caregivers were not confident in their ability to correctly administer home care. To address this, we recommended that the team at Northwestern Medicine create a series of instructional videos on how care should be administered when at home. This is information that is to be covered in appointments with clinicians, with the assumption that the videos will serve as an important resource to support home caregivers once they are actually involved in patient care.
There was initial push back at the cost of this endeavor, so we created a prototype to show them that this could be done at a low cost, and didn’t need to be a high production video.
Impact
The prototypes we created were very well received by our partners at Northwestern Medicine, so much so that they invited us to present them at their “all-hands” team meeting. They implemented all changes except the video prototypes into a dry run of their outpatient care model, and are still exploring avenues to acquire funding to create a high-fidelity series of instructional videos.